Rationale
In 2015, in anticipation of the launch of the Sustainable Development Goals (SDGs), the World Health Organization (WHO) and partners released a consensus statement and full strategy paper on ending preventable maternal mortality (EPMM). The EPMM target for reducing the global maternal mortality ratio (MMR) by 2030 was adopted as SDG target 3.1: reduce global MMR to less than 70 per 100 000 live births by 2030. WHO leads the United Nations Maternal Mortality Estimation Interagency Group (MMEIG) composed of WHO, United Nations Children’s Fund (UNICEF), United Nations Population Fund (UNFPA), the World Bank Group and United Nations Department of Economic and Social Affairs (UNDESA)/Population Division. The UN MMEIG is tasked with generating internationally comparable estimates of maternal mortality for the purposes of global monitoring, having done so for Millennium Development Goal reporting and will continue to do under the Sustainable Development Goals framework. Monitoring maternal health is widely seen as one of the most complicated health indicators within global frameworks. Significant unfinished business and challenges remain with estimating MMR; primarily due to the availability and usability of population based data on maternal death.
Definition
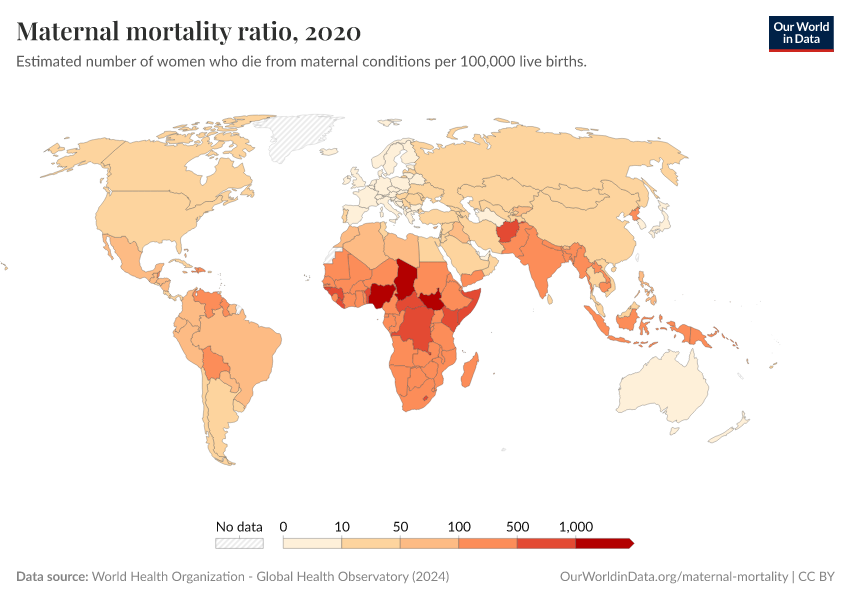
The maternal mortality ratio (MMR) is defined as the number of maternal deaths during a given time period per 100 000 live births during the same time period. It depicts the risk of maternal death relative to the number of live births and essentially captures the risk of death from a maternal cause in a single pregnancy (proxied by a single live birth). Maternal deaths (ICD-10): the annual number of female deaths from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes) during pregnancy and childbirth or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, expressed per 100 000 live births, for a specified time period. Maternal deaths are classified according to the International statistical classification of diseases and related health problems (ICD) definition. The specific codes used under ICD-10 (the 10th revision of the ICD) to define a maternal death are: O00-O96; O98, O99 and A34. ICD-11 (the 11th revision of the ICD) was adopted by the World Health Assembly in May 2019 and comes came into effect on 1st January 2022. Further information is available at: www.who.int/classifications/icd/en/. The coding rules related to maternal mortality are being edited to fully match the new structure of ICD-11, but without changing the resulting statistics. The ICD-11 rules can be accessed in the reference guide of ICD-11, at https://icd.who.int. Forthcoming releases from 2025 onwards will transition to use ICD-11 coding. Care has been taken to ensure that the definition of maternal death used for international comparison of mortality statistics remains stable over time, but the word “unintentional” has been used in the ICD-11 definition in place of the word “accidental” which was previously used, in ICD-10. Live birth: the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which, after such separation, breathes or shows any other evidence of life such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles, whether or not the umbilical cord has been cut or the placenta is attached. For the purpose of international reporting of maternal mortality, only those maternal deaths occurring before the end of the 42-day reference period should be included in the calculation of the various ratios and rates. The recording of later deaths is encouraged to inform national, regional, and global understanding of these events.
Method of measurement
The maternal mortality ratio can be calculated by dividing recorded (or estimated) maternal deaths by total recorded (or estimated) live births in the same period and multiplying by 100 000. Measurement requires information on pregnancy status, timing of death (during pregnancy, childbirth, or within 42 days of termination of pregnancy), and cause of death. Maternal mortality ratio = (number of maternal deaths/number of live births) X 100 000. The maternal mortality ratio can be calculated directly from data collected through civil registration and vital statistics (CRVS), household surveys or other sources. However, there are often data quality problems, particularly related to the underreporting and misclassification of maternal deaths. Therefore, data are often adjusted in order to take into account these data quality issues. Adjustments for underreporting and misclassification of deaths and model-based estimates should be made in the cases where data are not reliable. Because maternal mortality is a relatively rare event, large sample sizes are needed if household surveys are used. This is very costly and may still result in estimates with large confidence intervals, limiting the usefulness for cross-country or overtime comparisons. To reduce sample size requirements, the sisterhood method used in the Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS) measures maternal mortality by asking respondents about the survival of sisters. It should be noted that the sisterhood method results in pregnancy-related mortality: regardless of cause of death, all deaths occurring during pregnancy, birth, or the six weeks following the termination of the pregnancy are included in the numerator of the maternal mortality ratio. Two of the more common examples of specialized studies on maternal mortality are confidential enquiries into maternal deaths (CEMD) and reproductive-age mortality studies (RAMOS). CEMD refers to “a systematic multidisciplinary anonymous investigation of all or a representative sample of maternal deaths occurring at an area, regional (state) or national level which identifies the numbers, causes and avoidable or remediable factors associated with them”. RAMOS studies involve first identifying and then investigating and establishing the causes of all deaths of women of reproductive age in a defined population using multiple sources of data.
Method of estimation
Data on maternal mortality and other relevant variables are obtained through databases maintained by WHO, UNICEF, the World Bank Group, and UNDESA/Population. Data available from countries varies in terms of the source and methods. Given the variability of the sources of data, different methods are used for each data source in order to arrive at country estimates that are comparable and permit regional and global aggregation. The current methodology employed by the UN MMEIG in this round followed an improved approach that built directly upon methods used to produce the previous rounds of estimates published by the MMEIG since 2008. Estimates for this round were generated using a Bayesian approach, referred to as the Bayesian maternal mortality estimation model, or BMat model. This enhanced methodology uses the same core estimation method as in those previous rounds but adds refinements to optimize the use of country-specific data sources and excludes late maternal deaths. It therefore provides more accurate estimates, and a more realistic assessment of certainty about those estimates. The model still incorporates the same covariates which are: the Gross Domestic Product per capita based on purchasing power parity conversion (GDP), the general fertility rate (GFR), and proportion of births attended by a skilled health personnel (SBA). The UN MMEIG has developed a method to adjust existing data in order to take into account these data quality issues and ensure the comparability of different data sources. This method involves assessment of data for underreporting and, where necessary, adjustment for incompleteness and misclassification of deaths as well as development of estimates through statistical modelling for countries with no reliable national level data.